
Mark V., Chief Medical Officer
How we helped a major healthcare provider reduce readmission rates by 28% and improve operational efficiency by 31%

Mark V., Chief Medical Officer
A leading European healthcare network with 12 hospitals and over 3,000 healthcare professionals serving 1.5 million patients annually.
High patient readmission rates, inefficient resource allocation, and the need to improve preventive care measures while reducing costs.
Predictive analytics system for readmission risk, resource optimization platform, and AI-enhanced diagnostic support.
Reduction in readmission rates
Improvement in operational efficiency
Reduction in diagnostic errors
Annual cost savings
Our client, a major European healthcare provider, was facing significant challenges in their operations and patient care. Despite having skilled medical professionals and modern facilities, they struggled with high readmission rates, particularly for patients with chronic conditions. Their resource allocation system was largely manual and reactive, leading to inefficiencies in staffing and equipment utilization.
Additionally, the organization was under pressure to reduce costs while maintaining or improving quality of care. They had accumulated vast amounts of patient data but lacked the tools and expertise to extract meaningful insights that could drive improvements in preventive care and early intervention strategies.
"We were sitting on a goldmine of patient data but couldn't effectively leverage it to improve our care delivery. Our readmission rates were above industry standards, and we knew we needed a data-driven approach to address this issue at its root."
— Mark V., Chief Medical Officer
After a comprehensive assessment of the client's operations, data infrastructure, and specific pain points, we developed a three-pronged AI strategy focusing on predictive analytics, resource optimization, and diagnostic support.
We developed an advanced machine learning model that could identify patients at high risk of readmission. The system analyzed multiple factors including:
This system generated risk scores for each patient upon admission and continuously updated these scores throughout their hospital stay. High-risk patients were flagged for enhanced discharge planning and more intensive follow-up care.
We created an AI-powered resource management platform that:
The platform used reinforcement learning algorithms that continuously improved their recommendations based on outcomes and feedback.
We implemented an AI diagnostic support system that:
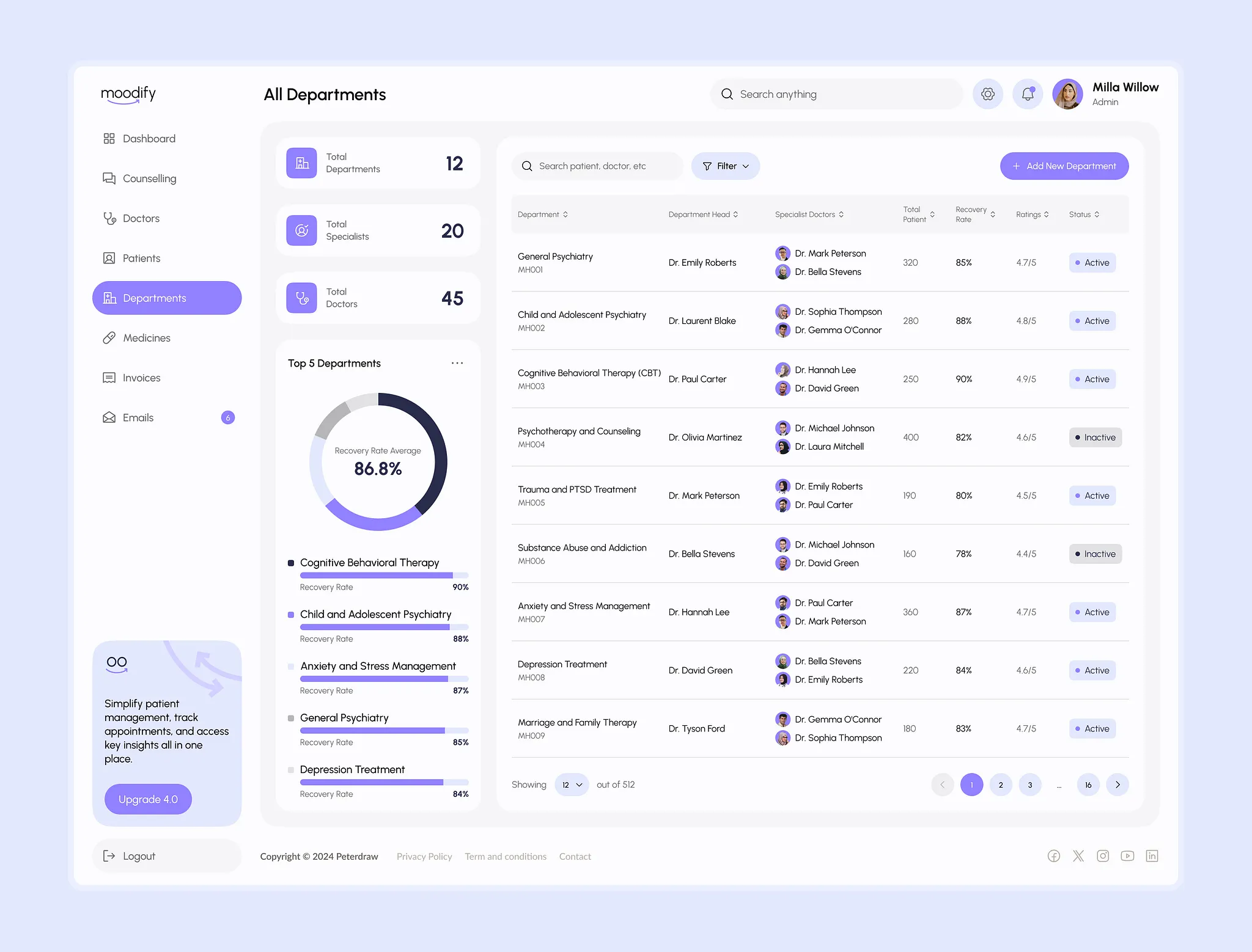
The predictive analytics dashboard showing patient risk stratification
We implemented these solutions through a carefully structured process:
Within 12 months of full implementation, the client experienced substantial improvements across all key metrics:
"The AI solutions implemented by ZeltAI have fundamentally transformed how we deliver care. The predictive analytics don't just help us react better to problems—they help us prevent them from occurring in the first place. Our staff now has more time to focus on direct patient care rather than administrative tasks, and our patients are experiencing better outcomes with fewer hospital stays."
— Mark V., Chief Medical Officer
Given the sensitive nature of healthcare data, we implemented several measures to ensure privacy and ethical use of AI:
This project provided valuable insights for healthcare AI implementations:
This case study demonstrates the transformative potential of AI in healthcare when implemented with a thoughtful, human-centered approach. By combining predictive analytics with resource optimization and diagnostic support, we were able to help our client significantly improve patient outcomes while reducing costs.
The success of this implementation has led to an expanded partnership, with plans to develop additional AI capabilities focused on personalized treatment planning and preventive care outreach programs.
Let's discuss how AI can improve patient outcomes and operational efficiency in your healthcare facility.